Pain, Posture, Proprioception and Performance
- Dr. E

- Apr 16, 2023
- 20 min read
Updated: Feb 11, 2025

Ok, this one is going to get a bit "heady" I apologize in advance. I had to write this just to hash things out in my own mind, really.
Over the past 4-5 years, there has been a hot debate about POSTURE and how it relates to pain and performance. Holy moly, has this become an ordeal. People in my industry start going at it over the trees and completely miss the forest, a majority of the time.
In the world of manual medicine, physical rehabilitation, and chiropractic there is more division than there is cohesion, that’s for sure. There are so many competing opinions about how to treat people, what we’re actually doing when we do treat people, what works, what’s a scam, what’s best at what time, and it goes on and on. I’m writing this article to make sense of it more, myself, and in that process hopefully, I will be able to communicate the important concepts to you.
Let’s start by tackling pain. It really is all in your head. After working with an estimated 5,000 unique patients, I can truly say it’s SUCH a subjective experience and is extensively multifactorial.

I know, that can be a bit triggering… and I would never discount someone's experience they are calling pain, however, the pain itself could be a software problem, kind of like a computer virus, not a hardware problem.
Briefly, let’s talk about 3 different receptor types our bodies use to perceive its environment.
Nociception is the body's process of detecting and responding to potentially damaging or harmful stimuli. This includes things like extreme temperatures, pressure, chemicals, and tissue damage. Specialized nerve endings in the skin, muscles, and internal organs, called nociceptors, detect these stimuli and transmit signals through sensory neurons to the spinal cord and brain for processing and response. Essentially, it's the system that helps us recognize a physical threat or harmful stimuli. This system is picked up in the brain and a response is determined by multiple factors.
Mechanoreception is the process by which the body detects and responds to mechanical or physical stimuli, such as touch or pressure. Similar to nociception, mechanoreceptors are specialized nerve endings in the skin, muscles, and joints that detect these stimuli and transmit signals through sensory neurons to the spinal cord and brain for processing and response.
Proprioception is the process by which the body detects and responds to changes in position or movement. This includes things like sensing whether a limb is in a certain position, detecting changes in spatial orientation, and maintaining balance and coordination. Proprioception relies on sensory feedback from specialized nerve endings within the muscles, tendons, and joints, which transmit signals through sensory neurons to the spinal cord and brain for processing and response.
These three processes are all related in the human body because they are all part of our sensory and nervous systems. They work together to help us navigate and interact with the environment, and to respond appropriately to different types of stimuli. We’re going to talk about proprioception a lot more in a bit.
There are no pain “receptors”
Pain is often thought of as a reflex. When you become “hurt”, the pain receptors send pain signals up to the brain and we sense pain, right? Nope. We don’t have ‘pain’ receptors.
As we just defined, these are the nociceptors at work. They are very similar to the other receptors which sense temperature, pressure, and chemicals. Nociceptors act more like “warning” signals, and they get stimulated when there is a noxious (damaging or potentially harmful) stimulus. Now, this is important to remember for later, tissue damage stimulates nociception, which in turn reduces mechanoreception and proprioception. Man, how about that for a tongue twister?
Pain is in your brain
When these ‘warning’ signals from the nociceptors reach the brain, your brain interprets them, decides whether a threat is significant or not, and then fires back varying levels of “pain” if necessary. To summarize, pain doesn't come from the stimulus, it comes from your brain's interpretation of the stimulus. This could explain the subjectivity and wide range of presentations. Pain is influenced by many factors including your thoughts, culture, stress levels, beliefs, and attitude.
Pain can change you
Acute pain due to trauma, surgery, and extensive tissue damage to a significant degree, usually goes away when the underlying injury has been treated or healed. It sometimes lasts for seconds, minutes, days, or weeks. But there are plenty of cases where pain persists even after the tissues have had enough time to heal. Pain that lasts for more than 3-6 months is termed chronic pain and has remained a mystery for many years.
We used to believe that your brain and nervous system could not change. In recent years, the study of neuroplasticity has shown that it absolutely can and does according to many different inputs and experiences.
We now know that persistent pain or pain which lasts for months and years can change the pain “pathways” to make them a lot more sensitive. And this hypersensitivity lowers the perceived threat threshold for any similar (or maybe not similar at all) stimulus.
It’s kind of like a skill that your body learns (which has pro’s and cons). When something has become chronically painful, oftentimes the tissue damage is no longer the source of the pain, it has now moved up into the nervous system and gotten kind of “lodged '' in there. Like riding a bike, it comes back pretty easily. This (sort-of negative) skill acquisition seems to be influenced by many other factors (like stress, fear, emotion, etc.) which explains the variability from person to person as far as its development. Also, as mentioned above, tissue damage (or maybe even just perceived tissue damage) stimulates nociception, which in turn reduces mechanoreception and proprioception.
So what can we do about it?
The role of any pain treatment should be to lower the threatening inputs. Just so that you know, we are talking about the treatment of chronic pain here and not acute pain (associated with tissue injury) which is pretty straightforward and well-understood.
What we are more concerned about is the chronic pain problem which has progressed beyond the normal healing time frame.
Bottom-Up Approach (Nociceptive - Hardware): This involves any treatments which lower or inhibit the nociceptive signals (bottom/hardware) to the brain (hence called bottom-up approach). Most current pain therapies targeting the tissues and joints are based on this ‘bottom-up’ approach. A simple example would be applying ice or heat to the damaged area. But these would also fall under this category:
Adjustments, myofascial therapies, EMS, ultrasound, etc. - and all come under this category.
Specific muscle imbalance, overactive/underactive corrective exercises.
Avoiding what caused the pain (i.e. lowering the weight you were lifting, modifying exercise selection, or just plain stopping with exercise/activities of daily living that you thought were contributing). More on this in a few paragraphs.
But the problem with this ‘hardware’ only approach is that the treatment is justified in a context that often reinforces the belief that there is something wrong in their tissues and joints (when maybe there no longer is), thereby raising the threat level, and potentially only providing short-lived temporary relief. The hardware is treated, but the software isn’t directly the focus, and could still have some "bugs".
Top-Down Approach (Non-Nociceptive - Software): This is done by educating the person about the physiology of pain, the role of the brain in pain, and “how pain does not mean harm” (hence we’re kind of hacking into the software - approach). This would be a software-first type of approach, decreasing fear, and slowly building resilience.
If we explain pain always as structural damage/defective hardware, every time people feel pain they perceive that they have re-injured, never fully healed, or something they’re doing is causing tissue damage (making them worse - ugh, if I had a nickel for every time I’ve heard “I just stopped everything because of the fear of making it worse” ). They start scouring their daily life for pain triggers and go to extreme lengths to rid their routines of pain-causing behaviors. They buy new pillows, posture braces, lumbar supports, beds, chairs, stand-up desks, cuss bosses, quit jobs, and drop booklets of FMLA paperwork on my desk. This thinking process heightens the threat level in the brain.. leading to pain persistence (fear-avoidance belief model).
The fear-avoidance model is now often seen as a central mechanism of how acute pain turns into chronic pain.
Pain education should encourage patients/clients to understand that “pain does not always mean harm”. Most of our current treatments based on the structural-pathology model may provide temporary pain relief, but pain explained based on our current model only helps to heighten fear of pain and anxiety in the patient.
When education about pain physiology is included in passive therapy (adjustments, physical therapy, etc.) treatment of patients with chronic pain, pain, and disability are reduced.
So, which is better?
Neither, for best results, we need to utilize both.
Gradual/Graded Exposure Approach or Activity: In this approach, the person is gradually exposed to feared activities without causing pain and thereby lowering the threat level in the brain, all the while rebuilding and/or maintaining physical capacity for said activities. These feared activities could be imagined movements, exercise, or daily functions.
Many researchers believe that a large part of pain relief seen with exercise and other rehabilitation methods is from lowering the threat level in the brain using the graded approach.
So when I convince my patients they need to get in the gym and take it upon themselves to start exercising and getting stronger they often come back later explaining they have considerably less pain, and they are often shocked by this. The software -softened-. The alert mechanism was dulled, and the hyper-reactive nature of the system has leveled back out to baseline.
Is it because they got stronger and more resilient? Or, were they just gradually exposed in a graded manner to the threatening movement/exercise? Probably both, but the latter is an important factor we can't underestimate.
Minimizing fear-avoidance and (re)building resilience via graded-exposure (when necessary) and intelligent physically imposed demands has become the central MISSION of my health and fitness coaching. - Dr. E
Let's look at a real-life example:
Meet Chris.
Chris is a pretty fit 36-year-old personal trainer. Chris hurts his low back doing deadlifts. He’s down and out for a few days, but within a week or so he's at least functional. He still has varying levels of pain dependent upon certain movements and physical tasks, but he's nowhere near as bad as he was for those couple of days.
Eventually, his severe pain has transformed into just a nagging ache, that can vary from a mild to moderate intensity, depending on the day/task. But now, every time he tries to even set up a deadlift he feels significant pain in his low back, and on his bad days sometimes just bending down to pick up his kids toys nearly drops him to his knees. He works in the fitness field and strongly believes that the key to getting stronger and bigger is performing big exercises like the squat and deadlift.
He runs to his local chiropractor for a couple of cracks that feel good, but the relief is short-lived. He gets an MRI that shows multiple disc herniations, gets a few injections from an orthopedic doctor, then begins physical therapy where he’s told his hips are uneven, his hamstrings are too tight, and his glutes “aren’t firing”. All this has convinced him he still has significant structural damage and faulty hardware. His pain has now dulled over the course of a month from a 9/10 to a 5/10. However, his beliefs, his attitude, and emotions have heightened the threat level in the brain and have made his nervous system a lot more sensitive to pain. He tries doing some light deadlifts but gets pain when he exceeds a certain weight, so he just gives up on deadlifting ("That's for the young guys, anyways”).
Fast forward 3-4 years and now he feels pain in the morning bending over the sink to brush his teeth, riding a bike or an elliptical, or doing anything related to his hips or low back for an extended period of time. Now he strongly believes his low back is very vulnerable to injury and he will never be able to deadlift or squat heavy again.
But because he’s a gym rat and still has an attachment to the way it made him feel when he could deadlift 3-400 pounds, he’s researching to see if it really is something that’s just in his past.
Now, things are looking up. His 4th chiropractor has finally explained to him that deadlifts aren’t dangerous, how complicated pain can be, how pain is an experience constructed in the brain, and how he may be dealing with “software” issues, more so than hardware, considering it’s been so long since his initial injury.
Software-Down Approach: He now clearly understands that the “broken-anatomy” model, which relies solely on the ‘bottom-up’, approach is incomplete. Just by understanding the physiology of pain or the ‘top-down’ approach, his threat level has lowered in the brain. He’s given himself permission to get into certain positions and exercises now, not thinking he’s aggravating his “broken anatomy” or faulty hardware. His nervous system is much less sensitive to pain and the brain finds no reason to induce pain because there is no threat and no action required. He feels much less pain now.
Hardware-Up Approach and Graded Exposure Method: He keeps seeing his chiropractor and diligently doing his corrective exercises, but now gradually starts incorporating deadlift variations and squats with light weights thereby lowering the nociceptive input (‘bottom-up approach’) and stays in a range that keeps him from flaring up. Within a few months, he is squatting and deadlifting, at his full capacity, with very little pain. He’s ditched his Chiropractor and only does a few of the corrective exercises.
Alright, so now we understand pain a little better.
If you’ve been told your pain is because of your posture, and you haven't done the necessary things to improve that posture, or maybe you don't even believe it can change, can you see how your software could be infected with a thought process that pain is never going away?

Okay, before we go down a rabbit hole on this one, let me explain how I feel about posture. It doesn’t exist. That’s all. Next topic.
I’m kidding, well... kind of.
I talk about "posture" all the time with my patients and oftentimes (because I’m busy helping lots of people) I don’t have time to go into this explanation, so I often give people quick cues and goals as far as “improving posture”.
What I should have said is that STATIC posture does not exist.
Sure, I assess what one would call static posture on every single patient, but it’s just a starting point for how people move and express themselves. Though as a collective we are a very sedentary culture, we're never completely still. If you're alive, it's impossible. Your heart is always beating, your rib cage is always expanding, blood is always pumping through your veins, and your body is always displaying a language.
So if you are a movement specialist, assessing posture in its most static position can give you an insight into how things go down when there is… more movement! It also can give you insights into how a person is feeling or expressing themselves if you're keen enough to pick up on it.
Amy Cuddy, a Phd social scientist, has some fascinating work in the area in the area of body language and relative mind-body-physiology changes. She's even written an awesome book called Presence, I read it long ago and loved it. Spoiler alert: she's found out that certain "power poses" (some may call these "postures") held for roughly 2-minutes can significantly impact one's testosterone and other hormone levels! Check out this brief synopsis highlight reel of her super famous (22.7 million views) Ted Talk if you'd like to see more about it.
"Orthopedic Vulnerability"
Keeping things focused on what most people seek my services for, I find myself explaining posture as your “orthopedic vulnerability”, or as I said, the starting point to how someone moves through their environment. The starting point from where you move is dynamic and always changing, hence there is no static posture. However, some people have adapted to "system defaults" that lead them to move a certain way, and in the vast majority of orthopedic injuries, repetitive, dare-I-say-faulty movement, is the precursor to injury and pain. It also clues us into a patient or client's movement habits to this point. It spotlights tight and tonic structures that could be playing a significant role in one’s motor dysfunction, injury, or movement difficulties.
So to recap, posture is a more static, expressive, phase of movement. When you have a deeper understanding of what it is, you understand that static posture doesn’t really exist. When you don't care to gain that level of understanding, it's an easy framework for people to understand, hence, why I still talk about it so often. What you should care more about is how you’re moving… and something else I call proprioception.

I’ve heard many practitioners and movement specialists refer to proprioception as our “sixth sense” as IT regulates your posture, not your chiropractor, and it’s the key to performance and longevity.
“If you break the word proprioception down, you get: perception of self. Proprioception is intimately linked to one of the basic types of intelligence: kinesthetic intelligence. One could argue (that would be me, in this instance) that kinesthetic intelligence is at the core of all the other forms of intelligence since it is with your physical body that you can experience any reality.” - Mat Boule, DO
Proprioception is where things get more important. So, if it’s our sixth sense, where/how do we sense it?
“Proprioception can also be entitled muscle sense. In order to know where you are in space without looking, your muscles are made up of receptors. These receptors are the muscle spindles. Muscle spindles are responsible for recording the length of a muscle. When a muscle is lengthened and when a muscle is shortened, it is sending less information to the central nervous system. In that context, we are less proprioceptive. What a bummer that is!
So it’s about sensitivity… of the muscle spindle, that is! The more sensitive the muscle spindle, the more you know where you are in space and the more you can recruit the muscular system for performance.” - Mat Boule, DO
Mat Boule is an Osteopath, Posturologist, and educator, and also has an awesome Ted Talk about posture. Some of his research is pretty fascinating, and the way he contextualized it in one of his talks really helped me understand it on a deeper level.
In the quotes above, he's basically saying the more sensitive your muscle spindles are, the better your muscles coordinate movement, and the better and more efficiently your body moves. This is critical, considering how we explained that how we move is where the majority of injuries occur or do not occur.
Guess where the highest abundance of these muscle spindles resides? Yep, you probably guessed it: the spine. These sensory receptors form a dense and highly sensitive network that maintains upright posture and responds rapidly to potentially damaging insults.
More particularly, the proprioceptive organs in the upper cervical (neck) region are particularly important in maintainging and collecting postural alignment, and in determining whole-body balance. The deep neck muscles have been found to have many more proprioceptive nerve endings than other skeletal muscles. They are very sensitive to changes in postural alignment and are a critical component (along with the vestibular system) in equilibrium and balance. In fact, researchers in a study were able to cause major changes in gait simply by anesthetizing the muscle and joint receptors in the neck.
The Bigger Picture
Proprioception’s impact goes a bit deeper than that though, I drew this diagram after listening to a presentation years ago. This presentation made my profession click for me. It finally explained the significance of what, we as chiropractors, are most influencing, and how it can have such profound effects.

Now, I don’t have a bunch of peer review papers to confirm all the mechanisms here, however, I can vouch that some really smart people, quoting textbooks and other really smart people, put this explanation together, not me.
So, I know this looks complicated, but I’m going to try to sum up that presentation in one quick video, here it goes:
Click the thumbnail to go watch the video, it's quick.
So now you understand the importance of this thing called proprioception.
Proprioception and Posture
"It just so happens to be that a proprioceptive deficit is a postural imbalance. The two simply cannot be separated. Posture is movement, and movement is posture." - Mat Boule, DO.
Now that we know that posture and movement cannot be separated, let’s look at it this way: movement is a succession of different postures. Essentially, if you break down movement, you get a series of flowing postures to achieve a certain physical performance.
Now that you’ve endured a few of my rants and basically slugged through a 4-year Kinesiology degree’s worth of information, let’s get to the nuts and bolts practical application here.
If we want to maximize proprioception, posture, movement, and quality of life, and minimize unnecessary pain, let’s connect some dots. In the next section, we’re going to explore how we were engineered to move.

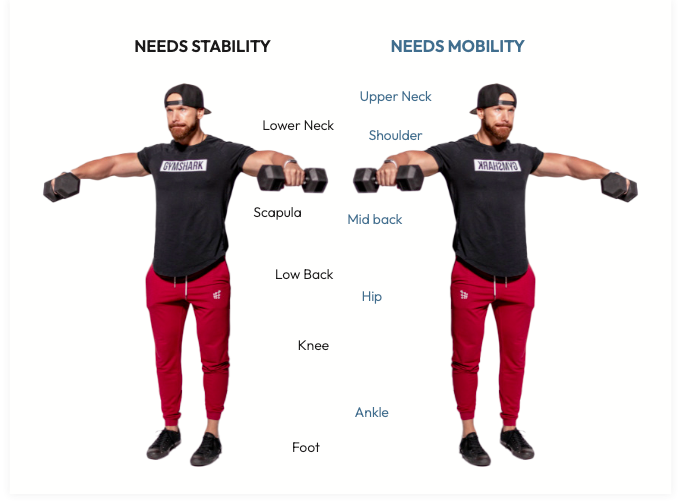
To tie this all up in a neat little bow, we need to look a little closer at our anatomy and how it’s so beautifully slung together. We are going to explore a concept coined the Joint-By-Joint model.
World-renowned physical therapist Gray Cook and fitness coach Mike Boyle shaped this concept based on their observations and history working with athletes. Understanding this concept has been an absolute game changer when it comes to how I treat patients and how I teach them to independently take care of themselves.
Each major joint in the body expresses both mobility and stability. Though they all express both, some joints are intelligently designed to prioritize one over the other to allow efficiency in global human movement. These tend to alternate up the movement chain. When you see the big picture, you see a stacked pattern of joints alternating between a primary function of mobility or stability.
Let’s briefly define a few terms to understand this a little better.

-Flexibility: describes the ability of the individual joint complex/muscle tissue
to move freely through its full range of motion with external help (passive range of motion, or how much somebody can "stretch" or move, with the help of someone else before tissue insult occurs). This is usually very different than "mobility".
-Mobility: describes the ability of the joint complex to move freely through its full range of motion without external help (active range of motion, or how much somebody can "stretch" or move, without the help of someone/something else before tissue insult occurs).
Anatomy 101 teaches us that certain joints should have a certain “normal” unassisted available range of motion. Any deviation from this norm would be what we consider a joint’s mobility relative to the average human norm.
Sometimes I consider "mobility" to be one's accessible active range of motion - For example, if something abruptly happens (a fall, an awkward step, or a reactionary movement of sorts) how far does a certain joint/muscle complex go before it damages or irritates tissue because of the demand exceeding the capacity. Mobility, in this light, very much depends on stability.
-Stability: describes the ability of a joint complex to maintain position (not move) without external help, while motion takes place somewhere else.
This is simply the ability to actively control or fix motion in one area while motion happens in another area. Stability can also be synonymous with the term motor control, and sometimes I just call it "active control".
Here’s why all this is important.
When a primarily mobile joint becomes immobile (because of trauma, sedentary behavior, stiffness, wear & tear, muscle imbalance, or altered mechanics), the primarily stable joint above or below will give up its stability and move (more than it would prefer to) as compensation. This is where things go haywire, mechanics get altered, and we start calling on certain anatomy to do stuff it doesn’t prefer to do. Movement breakdown occurs, injury ensues, and here comes our friend - nociception - that we’ve been talking so much about.
Let’s have a look at just how this pattern works its way through the whole body.
THE FOOT
Twenty-six bones make up the foot. It is a complex area of the body that has to carefully transmit ground forces up through the rest of the kinetic chain (subsequent joints upstream that achieve motion) It benefits from increased stability due to its tendency to become unstable during movement . All human movement is based on the foot. When the foot has a stability problem it will directly affect the rest of the chain (ankle, knee, hip, etc)
THE ANKLE
The ankle is an area of the body designed to be very mobile but tends to get stiff and tight and usually needs a lot of maintenance to maintain its mobility . The tendency for the ankle joint to become immobile affects the joints above and below, which are designed for more stability. If the ankle is lacking mobility, the mobility may have to come from one of those joints, thus potentially compromising it’s stability.
THE KNEE
The knee joint is designed to be more stable. Obviously, the knee is mobile and moves quite a bit during most athletic movements, but stability is the priority in this neck of the woods. When we move, we need to be able to control the knee. The knee must stay in proper alignment (stability) to avoid injury . Many injuries occur because the knee tends to bow in (valgus collapse) instead of staying aligned over the foot.
THE HIP
The hip joint is an area of the body that is designed for tremendous mobility. It’s a big “ball and socket” joint with many movement options. However, it tends to become stiff on most people (too much sitting, not consistently exploring the end ranges of motion, etc.) After a certain age, or after we discontinue a certain movement-related sport or practice, some people NEVER get their hips into full extension, as they would during a power walk or sprint. When was the last time you did? If hip mobility is compromised, it affects the ability of the joints above (low back - stability), and below (knee-stability) to perform their duties effectively and efficiently. Lack of hip mobility is nearly always a factor in lower back pain.
THE LOW BACK
The low back (lumbar spine & pelvis) has a priority of stability. Though there are many joints in the lumbar spine, they most need to be able to stiffen and maintain position while movement is happening elsewhere.
THE MID/UPPER BACK
The mid/upper back (thoracic spine) is a joint complex that requires mobility. This area of the body is inherently very stable due to something called a rib cage . The rib cage is attached here for the protection of our vital organs. Though inherently stable, this area tends to become even more stiff, stuck, and a little too stable. Hunchy postures, technology use, and sedentary behavior is usually the culprit here. Without thoracic spine mobility we increase our risk of compromising other upper body joint stability, which can lead to upper body dysfunction (leading to things like neck pain, back pain, headaches, shoulder impingement/injury, etc.)
The pattern works its way up through the scapula, shoulder, lower neck, upper neck, and can even be applied out through the upper extremity. It’s a beautiful system.
By understanding this model, and working towards training and maintaining the innate joint priorities, we can maximize movement efficiency, posture, and proprioception. Prioritizing mobility and stability in these areas will also reduce injury, nociception, and pain. I can personally vouch for this.
If you would like to learn more about this please go to www.elementxhfc.com and download my free Chiro-Companion Mobility Guide.
We went through a lot of stuff... Let’s recap:
There are no pain receptors, pain is your brain's interpretation of bothersome or potentially harmful stimuli transmitted to your brain by nociceptors, and that response can be influenced by MANY factors.
Noxious stimuli or tissue damage stimulates nociception, which in turn reduces mechanoreception and proprioception
Pain can hang around in neurology long after tissue damage/insult has fully healed, so understanding both the bottom up and top down pain relief strategies is critical for many chronic pain sufferers.
There is no static posture, as we are living beings and we are always moving.
Static “posture assessments” can give us great clues as to what is happening when people are moving, which is where the bulk of injuries occur.
Movement is a series of postures in succession
Proprioception is a sort of subconscious kinesthetic awareness of one’s body in space, and many refer to it as the 6th sense.
There is a lot of debate on whether posture matters or not, but when thinking about it critically, and understanding it is inseparable from proprioception and movement, it clearly does.
Proprioception, when optimal, has the potential to enhance the other 5 senses and can lead to better awareness of the environment and one’s needs.
Inflammation can lead to muscle/joint stiffness which can lead to a decreased level of proprioception, which can have farther reaching effects.
Proprioception, posture, and movement are all so closely related that they can pretty much be considered synonyms.
Understanding the joint by joint model, and optimizing your anatomy for how it was designed will lead to better posture, proprioception, movement, reduced nociception, and reduced injury.

The connection between pain, posture, and proprioception cannot be ignored when striving for optimal health and fitness. Pain is complex, but there are many ways to handle it, but giving up on the things that led to injury to begin with, is a bad idea. Utilizing graded exposure to return to similar activities, while building physical and mental resilience, is a much better strategy, and comes with many side benefits.
Posture is movement, and movement is posture. Optimal static postures don’t really exist, but our body definitely does have a unique and beautiful design that governs how it efficiently moves and expresses itself. Leveraging and understanding the joint-by-joint system can decrease nociception, and optimize proprioception. This in turn will allow us to move better, minimize injury risk, better sense our environment, and get more life per moment.
Here at Element X Health & Fitness Coaching, we take all these nuances into careful consideration as we provide personalized fitness consulting services to help individuals achieve their fitness goals, and get more life per moment.
We focus on three things over everything else:
effectiveness
efficiency
sustainability
If you would like to join the #fitlife movement, take action towards a healthy and pain-free lifestyle by scheduling a consult with our team, please apply here:
We’d love to have you join the fam, and help you transform your physique.
Until next time,
Health Disclaimer: The information provided in this article is for educational and informational purposes only. It is not intended to diagnose, treat, cure, or prevent any health conditions, nor should it be considered a substitute for professional medical advice. Always consult with your doctor or qualified healthcare provider before starting any new health program, making changes to your diet, taking supplements, or if you have questions about your medical condition. Your health decisions should be based on discussions with your healthcare team, not on the content you read online.







Comments